Diabetes Education Helped This Marine Vet Reach His Type 2 Goals
Editor’s Note: Get involved in Beyond Type 2’s #SeeTheSigns of diabetes campaign! Share your signs to help save lives, get sharable graphics for social media and more! Learn more here.
Garrett Reynolds is a retired marine gunnery sergeant of the United States Marine Corps. Diagnosed with type 2 diabetes in 2014, Garrett used the self-discipline skills he developed during his service to take action and control of his disease. By building positive habits and immersing himself in diabetes self-management education, he’s found a way to live become his healthiest self. Garrett now uses his voice to speak about living with type 2 diabetes and how people with type 2 can empower themselves through diabetes education.
When were you diagnosed with type 2 diabetes? What symptoms did you have?
I was first diagnosed in June of 2014. I had all of the symptoms—my eyes were starting to get blurry; frequent urination; shaking. To be quite frank with you, I thought it was an issue with my colon at first because I couldn’t understand why I had to use the bathroom so much. I was going to the bathroom about 20 times per day. Because of what was happening, I probably had diabetes for a year and didn’t even know it.
I couldn’t even go to the movies and watch the whole movie or sit through dinner without having to excuse myself to use the bathroom. My wife and I decided I needed to get checked out. When I did, the nurse asked me if I had diabetes, to which I responded no. I insisted something was wrong with my colon. She then asked if I’d ever had my blood glucose checked and my answer to that was no. When she checked my blood sugar, it was 24.3 mmol/L438 mg/dL. The nurse gave me a frightened look and said my blood sugar should be around 5.0 mmol/L90 mg/dL—but I didn’t know that; I didn’t know what 24.3 mmol/L438 mg/dL meant. Instead of letting me go home, she said I needed to go to an emergency room and receive medications immediately.
My wife drove me to the emergency room. After I told a staff member what my blood sugar was high, they ushered me in and said I was in danger of falling into a diabetic coma. I was hooked up to an IV and a doctor confirmed I was a type 2 diabetic. They wouldn’t let me go home until my blood sugar was lowered to safe levels. To start, I was given six units of insulin. That wasn’t enough, so they gave me another six an hour later. That still wasn’t enough; I was at 15.6 mmol/L280 mg/dL. It took one more shot of insulin for it to come down to a level where they would let me go home. In total, I was given 18 units of insulin. When I left, they gave me a prescription for 1000 mg of metformin. That day, I remember being a little tired, fatigued and a little scared. This was a life-changing event. Later on, I found out my A1c was 14.6 which was, according to them, literally off the charts. Their chart only went up to 12. It was both comical in one sense and frightening in another.
What risk factors do you think were at play?
The way I ate. Even though I ran and lifted weights, I thought it wouldn’t be an issue with me eating whatever I wanted to eat. I was in denial about it. So when I first was diagnosed with diabetes, I started learning about carbohydrates, proteins and fats. I started taking diabetes education classes immediately at the hospital. I wanted to read as much literature as I could and educate myself quickly because I realized that this was a life or death situation. This had to be taken very seriously.
Was the diagnosis a surprise? Does it run in your family?
No, it doesn’t run in my family. I was ashamed when I was first diagnosed. I couldn’t believe I’d been diagnosed with diabetes. It’s something that I heard people had and there’s the stereotype of what a a person with diabetes looks like. I was wondering why this was happening to me. I had to come to grips with what was occurring, including learning about this diagnosis and what I had to do to change my lifestyle. I also had to think about how my decision was going to affect not only my life but the lives of my family and friends.
For the first couple of months, I was in denial and didn’t tell anyone about my diagnosis. I felt I cheated myself by not eating right or being educated enough to know what I was consuming. I began to learn about food and carbs, meal planning and read food labels. I watched a lot of videos on how food is digested by the body and turned into glucose.
I also thought about losing limbs. When I was young, a lot of people I grew up with in Chicago would say this person had “sugar” and they would lose a finger or a toe because of diabetes. And even in the movie Soul Food, for example, the grandmother was burning her hand over the stove without realizing it because she had diabetes. After that, I told myself I had to make an effort and move forward. That was my motivation to change the course of my life. Even though I didn’t want anyone to know about my diabetes, in the beginning, I’m more open about it.
What is your diabetes regimen like now?
I changed my diet to the point where I’ve eliminated a lot of foods that are absolutely okay to eat, but I’ve done it because I want to get so ahead of this disease. For example, I used to eat a lot of pasta. But now, I don’t eat as much as I used to. I used to eat beef, especially burgers, but not anymore. Seafood is my main source of protein. As good as they are, I don’t eat hot dogs or bacon anymore. I eliminated high fructose corn syrup from my diet and drink more water now. If I drink soda, I look at the label to see if it has natural sugar in it and no high fructose corn syrup. It’s bad for you and it’s in almost everything. I’ve mostly removed alcohol from my diet, with the exception of the occasional glass of wine.
Other than metformin, I’m on 20 mg of simvastatin to manage my cholesterol, and 40 mg of lisinopril for my heart. Since I was diagnosed, I’ve made sure to go see my doctor and get my blood work done at least every four months. My doctor has been so excited about my progress and said I’ve come so far and said I have my diabetes under control. He called me a success story because I’ve been able to manage it with medication and my lifestyle.
Also, though, I see a private family physician, my prescriptions are covered by my VA benefits due to my status as a retired serviceman.
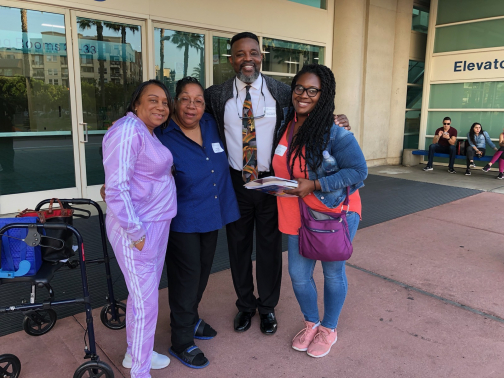
At the TCOYD conference in San Diego, Dr. Steve Edelman, the founder and director of the organization, asked me to speak at the closing session. I want to be someone who helps other people before they become diabetic and to be proactive about diabetes. We should be standing up for diabetes. Stand up tall and say yes, this disease impacts a lot of people and it’s nothing to be ashamed of. It’s almost like a mental health problem that comes with the stigmas of diabetes.
There’s a lack of education about type 2 diabetes and that’s what we need. And education is what I’ve chosen to use to help me. I’m a huge advocate of talking about it any chance I get and I don’t mind sharing my story with anyone because I’m still living the story. It’s not over, it’s ongoing.
You mentioned your work with vets, do you speak to them often about this issue? How many vets with diabetes have you come across?
Great question. I do speak with vets every single day. I work on Camp Pendleton and I’m a senior analyst for a company called CodePlus. It’s a company based out of Fairfax, Virginia, and I’m a satellite employee who works here in California. I work on-site with the Marines. I’ve been out on this particular base at Camp Pendleton for the last 14 years working in concert with the Marines with their weapons systems that they employ overseas to fight the war on terror.
I’m very open about my diabetes. I let them ask me any questions. Someone would inquire about my diabetic bracelet, tell me they have a family member who has diabetes and will ask for more information about it. I’ve spoken to several active duty service members about it. I’ve encouraged them to get diabetes education because the best one I received was Tri-City Medical Center in Oceanside, California. It was a free class and they gave you a meter.
Did your experience in the Marines help you control your diabetes?
The discipline and spirit that I learned while I was active duty have helped me to identify this is an issue that needed to be taken care of. From 1986–1989, I was the senior drill instructor in San Diego and used to train the recruits coming out of high school or that are in college who wanted to be Marines. It was 30-something years ago, but I still maintain that motivation and discipline that I had then. I wake up with the same exuberance and motivation to want to make an impact every day.
We teach our recruits to be responsible for their actions. I hold myself to the same standard. I told myself, “Okay Garrett, you’ve got to be responsible for your actions and you have to take hold of this and not let this defeat you.” None of us will make it out of this life alive; we’re going to die of something at some point. But the quality of your living is what’s important. Why are you living?
Have you thought about wearing a continuous glucose monitor (CGM)?
No. I haven’t considered that. At the TCOYD conference, I got the chance to see more of that. They were presenting more of that. And I don’t, at this point, I’m okay with the finger prick. It hasn’t gotten to the point that it bothers me enough to wear a device full time.
What are some misconceptions about type 2 diabetes that you think people have?
Misconceptions are that people with type 2 diabetes are overweight, lazy and don’t work out. You’re stereotyped as a person who doesn’t look out for your own best interests when it comes to your body. People assume you don’t take care of yourself. That’s why I was so embarrassed when I was diagnosed because I was taking care of myself. I was running, exercising and lifting weights. But I would eat whatever I wanted. I didn’t think anything of it because if I was going to the gym the next day, what’s the problem? But one thing I learned through that is you can’t work out a bad diet.
What are some words of empowerment you have for our audience?
Education, education, education. Learn as much as you can. Come to grips that this is a real diagnosis that is life-changing. You have to be the person who does what’s in your best interest. Submerge yourself in knowledge about diabetes. What does that mean? It means to go to the conferences. Go to the library and take out a book on diabetes. Go to websites to learn how this disease progresses. When I got on stage [at TCOYD], I said this diagnosis was the best thing that happened to me. It has made me more aware of what I eat.
How do you live #BeyondPowerful with diabetes?
I’d say with prayer. I am a Christian, so I have instilled beliefs in God and our creator. My motivation also is when I get up in the morning and I take my blood pressure and blood sugar. When my numbers show I’m doing well, I remain motivated.
Recently, my doctor told me my A1C was 6.4 or 6.6. I don’t want to cheat myself or the people who love and care for me. And then, let’s help other people. Through the grace of God, we’ve been able to have the knowledge and education to make us better. Our generation has been a beneficiary of all of the knowledge and the latest interventions for type 2 diabetes. We’re at a point now where we have so much information about type 1 and type 2 diabetes that we should be able to care of ourselves.
I’m standing up for diabetes education and personal wellness Marine Corps style! Ooorah!